McLaughlin Research Institute scientists develop assay to detect protein misfolding in amyotrophic lateral sclerosis (ALS), also called Lou Gehrig’s Disease
Dr. Moses Leavens, assistant professor at the McLaughlin Research Institute and the Touro University – Montana campus, and his colleagues have developed an assay to detect protein misfolding in amyotrophic lateral sclerosis (ALS), also called Lou Gehrig’s Disease. Dr. Leavens grew up in Great Falls, MT, and attended area universities for his education. He received an associate degree from Montana State University – Great Falls College, his Bachelor of Science from the University of Providence and his doctoral degree from the University of Montana before completing postdoctoral research at the Rocky Mountain Laboratory in Hamilton, MT. He has experienced a breadth of experience in Montana that prepared him well for his latest work.
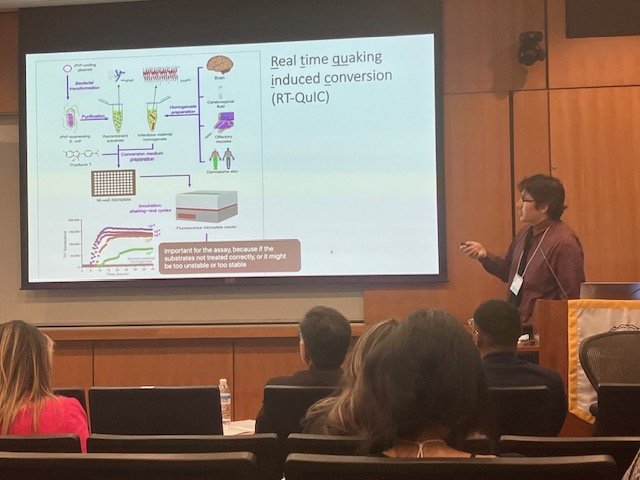
Lou Gehrig’s disease is named for the famous Yankee baseball player who died from ALS in 1941. ALS is an especially rapidly progressing neurodegenerative disease, with an average lifespan of just 2–5 years after diagnosis. New ways to diagnose the disease are much needed if early diagnosis and treatment is to be a possibility. Dr. Leavens worked with colleagues at the McLaughlin Research Institute (Justin K. Mielke, Mikael Klingeborn, Erin L. Markham, and Emily D. Reese), the University of Montana (Eric P Schultz), the Rocky Mountain Laboratory (Parvez Alam and Byron Caughey), the University of British Columbia (Ian R. Mackenzie and Neil R. Cashman) and at Washington University in St. Louis (Cindy V. Ly) with the goal of identifying new prognostic and pharmacodynamic biomarkers that would allow diagnosis of ALS and predict disease path or course. Dr. Leavens and colleagues focused on a protein called superoxide dismutase 1 (SOD1) which is known to accumulate and form insoluble clumps or aggregates in ALS patients who have a mutation in their SOD1 gene. Interesting, this research shows that aggregates of SOD1 are detected in genetic (familial) cases but also in sporadic forms of the disease where no genetic cause is known. The results of the studies indicate that SOD1 seeds may provide a useful diagnosis for ALS patients across a spectrum of severity and causes. Indeed, SOD1 seeding or aggregation activity is a promising biomarker, particularly in sporadic ALS cases for whom no genetic testing is currently available.
Dr. Leavens and colleagues will continue to develop this work towards clinical applications in ALS and also in other neurodegenerative diseases such as frontotemporal dementia, Alzheimer’s disease and Parkinson’s disease.